Male Infertility
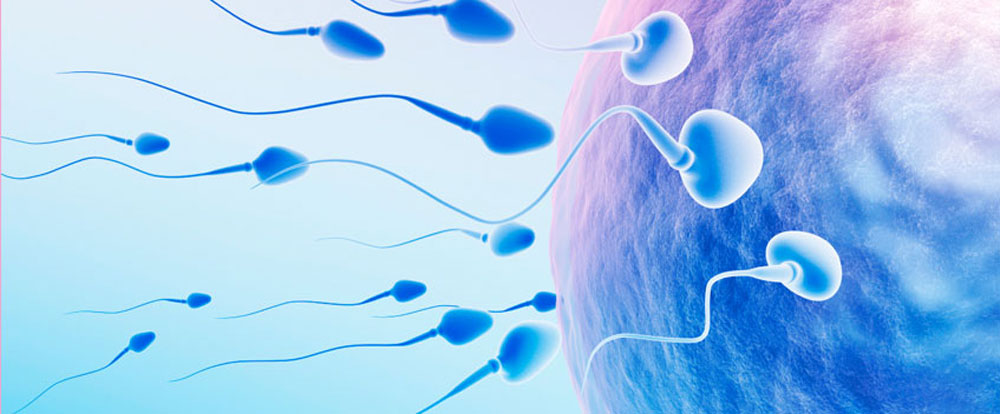
Approximately 25% of all infertility is caused by a sperm defect. About 40-50% of infertility cases have a sperm defect as the main cause, or a contributing cause. This is the legacy of male factor infertility. It can be difficult to know whether sperm is the sole problem, or just a contributing cause of infertility. Partly this is because 'numbers are just numbers'. For example, we know that men with very low sperm counts can sometimes have children - and some men with normal sperm counts can be infertile. What matters most is not how many sperm there are or how fast they swim - but whether they can fertilize the female partner's eggs. Sperm defects are a biochemical issue at the molecular level. A sperm defect is present when sperm are irregularly shaped, have poor motility or low sperm count. It takes more than looking at sperm under the microscope to assess the ability of the sperm to fertilize the female's eggs. In nearly 40% of all infertility cases the cause is attributed to the male. In the cases of male factor infertility, more than 90% of the time it is caused by poor sperm quality. Other causes of male infertility may include anatomic, hormonal or genetic imbalances. Less than a decade ago, treatment for a severe male factor infertility was limited to inseminations or IVF using donor sperm. Today, significant advances in male infertility have introduced innovative therapeutic options that offer men, including those with no sperm in their ejaculate due to genetic conditions, a greatly improved chance to conceive their own biological offspring.
Male infertility treatment
Sperm Retrieval
This technique is used to help couples where the male partner does not ejaculate sperm. A small number of sperm are obtained directly from the epididymis or testicles in a small surgical procedure sufficient for IVF treatment.
Percutaneous Epididymal Sperm Aspiration (PESA):
The procedure is usually done under sedation with pain relief, but can be done under General Anaesthetic
In some men, sperm can be extracted directly from the epididymis
A fine needle is passed through the skin of the scrotum and placed in the epididymis
Small amounts of fluid can be taken and examined for sperm alternatively;
Testicular Sperm Aspiration (TESA):
Sperm is extracted directly from the testicles by passing a fine needle directly into the testicle
A small amount of tissue is extracted and prepared in the laboratory and examined for sperm.Sperm obtained are either frozen for subsequent use or prepared using a process of washing and grading. A single sperm is then injected directly into each egg in a process known as intracytoplasmic sperm injection or ICSI.
Reproductive Surgery
When non-surgical and natural remedies fail to improve male fertility, surgical options are the key to fulfill the dream of having children.What is nice about surgical treatments for male infertility is that they can “cure” the problem and allow for conception at home and not in the laboratory.
1. Varicocele Repair -
Varicoceles are enlarged varicose veins that occur in the scrotum. They are fairly common, affecting 15 out of 100 men overall and 40 out of 100 men with known infertility. Varicoceles occur most often in the left testicle. Varicocele repair is done to improve male fertility. It can usually be done surgically on an outpatient basis using local or general anesthetic. A small incision is made in the abdomen close to where the testicles originally descended through the abdominal wall. The veins that produce the varicocele are identified and cut to eliminate blood flow to the varicocele.
2. Ejaculatory Duct Resection -
Ejaculatory duct resection presents with a low ejaculate volume on semen analysis in association with no sperm count or very low sperm motility. Ejaculatory duct resection is the cause of infertility in 1-5% of infertile men. Although unusual, ejaculatory duct resection is diagnosed and treated with minimally invasive techniques.
3. Vas Deferens or Epididymal Blockage -
The male reproductive tract is basically one long tube of varying dimensions. Infection or traumatic injury to the genital tract can result in scarring and blockage within this tube. A classic example of a surgically correctable blockage is a vasectomy. Approximately 5% of men who have a vasectomy undergo a vasectomy reversal. The success of a vasectomy reversal depends on many factors, the most important of which are the skill of the surgeon and the findings at the time of surgery. In the best of circumstances, 85-99% of patients can be expected to have a return of sperm after vasovasostomy (vas to vas connection). With a healthy female partner, this is associated with a pregnancy rate of 60-65%. The surgery is performed as an outpatient and the patient is generally able to return to work in 3-4 days. When congenital absence of the vas deferens is diagnosed, microsurgical reconstruction is generally not possible; however, sperm extraction techniques can be offered to patients.
4. Vasectomy -
Vasectomy, a form of male sterilization utilizing bilateral disruption of the vas deferens to halt the transmission of spermatozoa during ejaculation, is an outpatient procedure that can be performed in the office setting under local anesthesia, with most patients reporting only minimal postoperative pain. Unlike many of the other methods of contraception, which require continuous usage or repeat administrations, vasectomy needs to be performed only once for a man to be rendered durably sterile. Despite advances in other methods of family planning during the last several decades, vasectomy has remained among the most popular forms of contraception. The safety, simplicity, and durability of the procedure make it an attractive option for patients and physicians alike.